PORTLAND, Ore. — Washington Governor Jay Inslee signed legislation Tuesday to end surprise medical billing.
The new law, which takes effect starting January 1, 2020, protects Washington consumers from unexpectedly large medical bills after they go to the hospital.
Surprise bills often come from emergency room doctors or hospitals that are outside a patient’s insurance network.
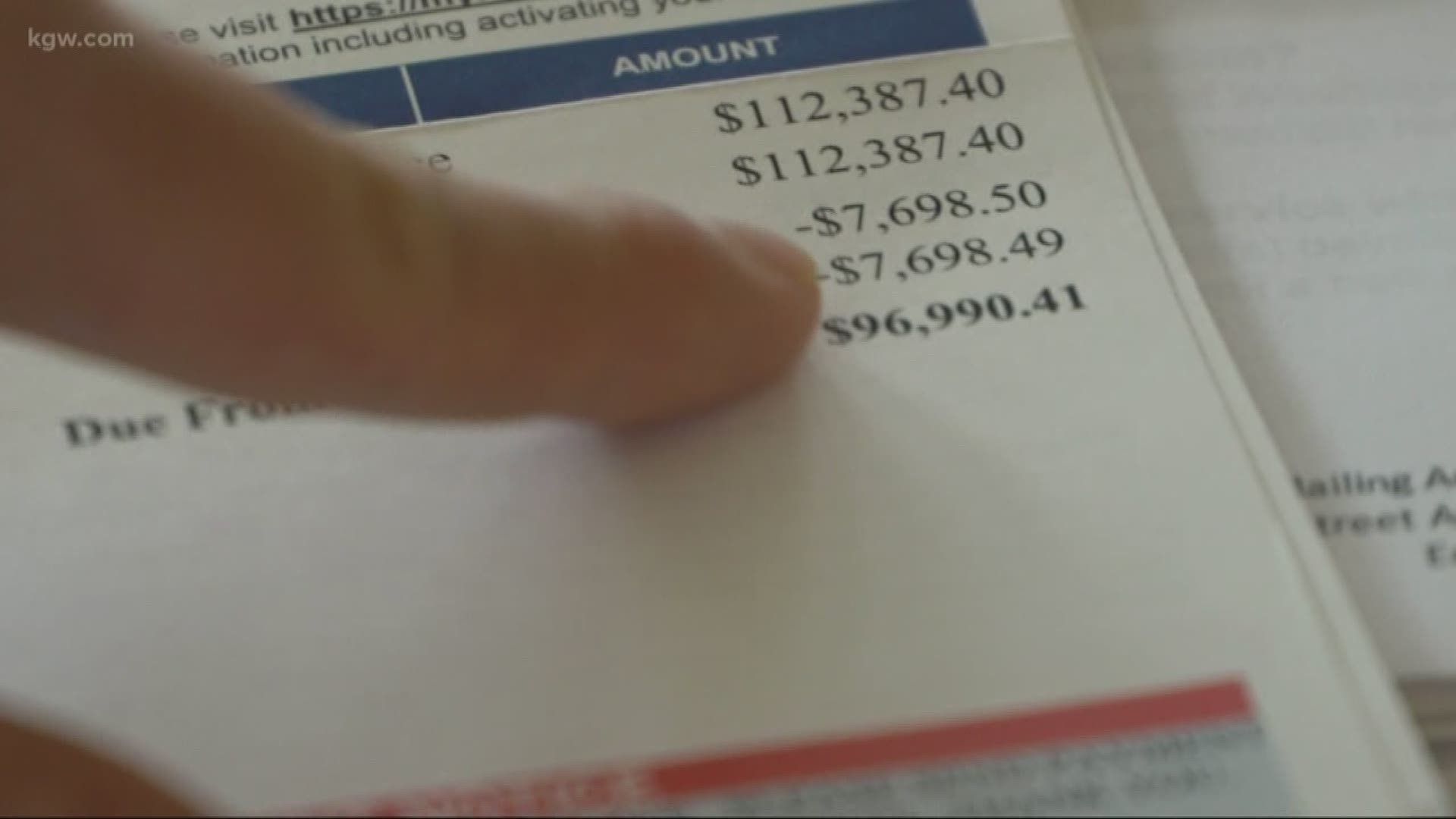
Jaime Hansen of La Center attended the bill signing ceremony in Olympia. Last year, Hansen received a surprise medical bill for $96,000 for her son’s emergency care at a Portland hospital. Her insurance company, LifeWise Health Plan of Washington would only cover a small portion of the bill because the hospital was out-of-network.
Insurance Commissioner Mike Kreidler intervened and helped reduce Hansen’s bill to roughly $24,000. Hansen testified before House and Senate committees in Olympia in support of legislation protecting consumers from getting a surprise bill.
“When something is wrong, you have to speak up,” said Hansen. “I think this law is going to have a huge impact.”
Kreidler added, “I think the breadth of these stories – and that no one was immune – finally provided the motivation needed for the sides to come together and find a solution.”
The Insurance Commissioner outlined key protections:
- A consumer who receives emergency care in an out-of-network emergency room or who has a non-emergency medical procedure in an in-network hospital or facility cannot be balanced billed.
- An insurer cannot balance bill a patient if they seek emergency care at an out-of-network facility in a state that borders Washington.
- Insurers must pay the out-of-network provider or facility directly for care their enrollee receives.
- If the insurer and provider or facility do not agree on a commercially reasonable payment for out-of-network services within 30 days, their dispute goes to binding arbitration.
- A disclosure template will be developed and must be given to patients describing when they can and cannot receive a balance bill.
- Insurers, providers, and facilities must include up-to-date network information on their websites.
- Any provider who continues to illegally balance bill may be referred to the state Department of Health for enforcement.